Understanding What Makes This Approach Different
At its core, the shared decision making model is about the fundamental difference between being told what to do and being asked for your input. It marks a significant departure from the traditional, paternalistic “doctor knows best” attitude. Instead, it creates a partnership where the healthcare provider acts as a trusted advisor, helping you sort through complex choices to find what works best for your life.
This isn't just about good manners; it's about acknowledging that patients have irreplaceable expertise. You are the expert on your own life, values, and circumstances—knowledge that no amount of medical training alone can replace.
This shift toward partnership has seen a massive surge in interest. When the first major international conference on this topic took place in 2001, only 73 publications on PubMed even mentioned the term. By 2022, that number had exploded to approximately 2,300 publications in a single year. This growth shows just how seriously the medical community is taking this collaborative approach.
From Monologue to Dialogue
The old way of doing things often felt like a monologue, where a clinician delivered a diagnosis and a prescription with little back-and-forth. In contrast, the shared decision making model fosters a true dialogue. It’s a collaborative space where clinical evidence and a patient’s personal expertise carry equal weight. This creates a more balanced and respectful dynamic, moving beyond simple patient compliance to achieve genuine teamwork.
Some common misunderstandings can prevent people from embracing this model. A frequent concern is that it might diminish the clinician's expert role or place too much responsibility on the patient. However, the goal isn't for you to make the decision alone. It’s about creating a plan together by merging professional medical knowledge with your personal autonomy and life context. This balance is key to making choices that are not only medically sound but also practical for you.
The diagram below shows how information and preferences flow between a patient and clinician during a shared decision making conversation.

As the visual shows, it’s a two-way street. Both parties contribute essential information, discuss the options, and work toward a consensus—a big change from a top-down directive.
Real Stories, Real Impact
The real power of this model comes to life in stories from patients and providers.
- A patient with multiple chronic conditions might work with their doctor to prioritize treatments that fit their goal of staying active.
- A newly diagnosed cancer patient can discuss treatment side effects with their oncologist in the context of their family life and job.
These conversations result in care plans that people are more likely to understand, believe in, and stick with. This collaborative spirit is what makes the shared decision making model a true advancement in modern healthcare, improving both health outcomes and patient satisfaction.
The Three Essential Elements That Make It Work
Imagine the shared decision making model as a sturdy, three-legged stool. If you take away even one leg, the whole thing topples over. For a healthcare experience to be genuinely collaborative, all three core elements must be present and working in concert. These components elevate a typical medical visit from a simple information exchange to a process of co-creation.
This infographic shows the key steps a clinician and patient navigate together, highlighting the partnership at the core of the shared decision making model.
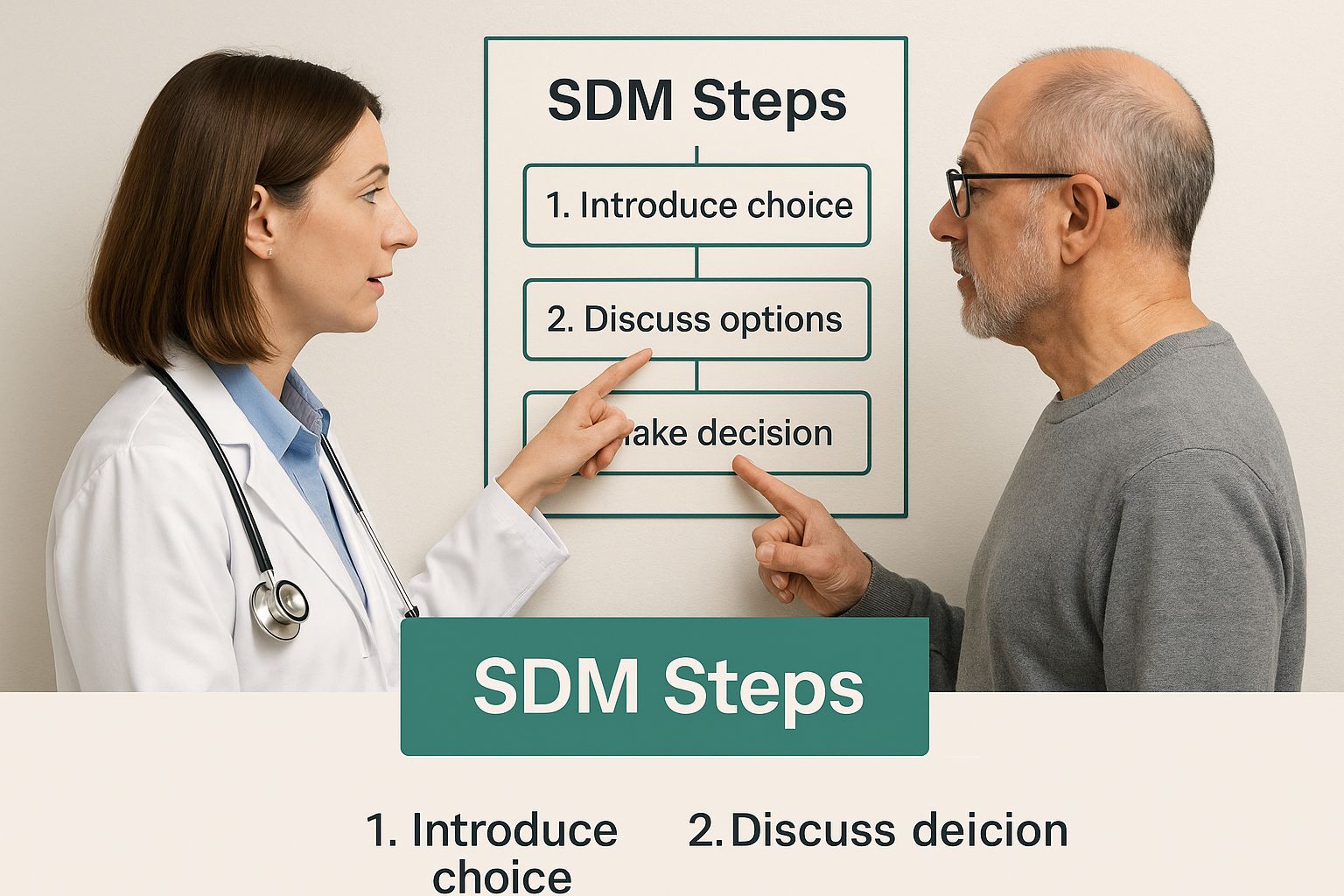
As the image illustrates, the path forward involves a joint effort, with both parties actively working towards a mutual understanding and outcome. Let's look at the three legs that support this entire process.
To better understand how these elements function, it's helpful to see how they differ from a more conventional approach.
| Component |
Traditional Approach |
Shared Decision Making Approach |
Key Benefits |
| Information Sharing |
The clinician delivers facts and medical jargon. It's often a one-way flow of information. |
The clinician acts as an interpreter, translating complex evidence into understandable options relevant to the patient. |
Clarity and Relevance: The patient understands what the options mean for their life, not just the clinical data. |
| Deliberation |
The patient is expected to listen and ask clarifying questions. The focus is on the clinical problem. |
A two-way conversation where the patient's values, goals, and life context are combined with clinical facts. |
Personalization: The final choice is tailored to the patient's unique circumstances and priorities. |
| Decision |
The clinician often recommends a single "best" option, and the patient agrees or disagrees. |
The clinician and patient jointly arrive at a mutually agreed-upon plan after weighing all factors together. |
Empowerment and Buy-in: The patient feels like an active partner, leading to higher confidence and adherence. |
The table makes it clear: shared decision making isn't just a friendlier version of the old model. It fundamentally changes the roles and the conversation to produce better, more personalized outcomes.
1. The Right Information at the Right Time
The first leg of the stool is information sharing, but this is much more than a one-way data dump. In a standard appointment, a doctor might rattle off facts and statistics in dense medical terms. In shared decision making, the goal is translation, not just transmission. The provider’s job is to be an interpreter, turning complex clinical evidence into clear, relatable insights.
This means discussing:
- The nature of the diagnosis in plain language.
- The complete set of reasonable treatment choices, which includes the option of "watchful waiting."
- The potential upsides and downsides of each choice, framed in a way that connects to the patient’s actual life.
For instance, instead of only saying a medication has a “20% chance of side effects,” a provider would explain what those side effects feel like and how they might interfere with the patient’s daily life, such as their ability to drive or care for their family.
2. Deliberation: The Heart of the Conversation
The second leg is deliberation, the back-and-forth dialogue where the patient’s expertise truly shines. This is where clinical facts intersect with real-world context. While the clinician provides medical knowledge, the patient contributes essential wisdom about their own life, including their personal values, life goals, fears, and available support systems.
During this phase, the conversation evolves from "What are the options?" to "What do these options mean for you?" A provider might ask questions like, “You mentioned wanting to travel next year. How would this recovery timeline impact those plans?” or “How important is it for you to avoid treatments that might make you feel tired?” This careful deliberation makes sure the final choice fits the patient’s personal priorities, not just medical guidelines.
3. Reaching a Collaborative Decision
The final element is the collaborative decision. After transparent information sharing and thorough deliberation, the patient and provider reach a treatment plan they both agree on. This decision is never rushed; it’s the natural result of a process founded on trust and mutual respect. The patient should feel empowered and confident, understanding the "why" behind the chosen path.
Getting buy-in from the person who has to live with the decision is a recipe for success. This collaborative agreement changes the patient from a passive recipient of care into an active, engaged partner in their own health, which is the ultimate goal of the shared decision making model.
Why People Are Choosing Partnership Over Paternalism
A major change is happening in healthcare. The old way—where a doctor's word was the final say, often called paternalism—is being replaced by a more cooperative method. People seeking care today are not just passively accepting instructions; they want to be active partners in the decisions that affect their health and well-being. This shift is fueled by easier access to information and a growing desire for personal control.

This trend isn't just a feeling; it's backed by clear data. When offered a choice, patients show a strong preference for being more involved. Recent studies highlight that around 71% of patients would rather have a shared or patient-led style of decision-making than the traditional, clinician-directed approach. This significant number shows a fundamental need for collaboration in modern healthcare. For more details on these findings, you can review the patient preference research from the JAMA Network.
Why Is This Shift Happening?
The move towards partnership has several roots, offering advantages for both patients and medical professionals. It's a clear acknowledgment that the clinically "best" choice isn't always the right one for a person's life.
For Patients: A Voice and a Choice: The shared decision making model gives patients something incredibly important: the sense of being genuinely heard and respected. When they participate in creating their own care plans, patients feel more confident in their treatment paths. They are no longer just following a script but are co-authoring their health story. This feeling of ownership leads directly to better follow-through on treatment plans and, ultimately, better health.
For Providers: A More Rewarding Practice: Clinicians also find this new dynamic beneficial. Using the shared decision making model can make their work more fulfilling by building stronger, more trusting relationships. It helps prevent the conflicts that can pop up when a patient feels their perspective has been ignored. With medical treatments becoming more complex, it’s impossible for one provider to know what is most important to every single patient. This partnership allows them to recommend treatments that are both medically sound and manageable for the individual. By sharing the responsibility of a decision, providers can be sure the final plan has the patient's complete buy-in, making it much more likely to succeed. This turns healthcare from a transactional process into the foundation for lasting, effective health partnerships.
Making It Happen: A Practical Implementation Roadmap
Knowing the principles of the shared decision making model is one thing, but successfully weaving it into the fabric of a busy healthcare setting is another challenge entirely. The journey from a top-down system to a collaborative one requires more than good intentions. It demands a structured, phased approach that addresses workflows, tools, and the very human side of change. This isn't just about teaching better communication skills—it's about redesigning how care is delivered to create time and space for meaningful conversations.
A successful rollout isn't a single event but a continuous process of improvement. Organizations that get it right often borrow from frameworks that emphasize testing and learning, similar to the methods seen in agile business development. You can explore these concepts further in our guide on lean startup principles for building successful ventures. This mindset helps healthcare systems adapt to the unique needs of their patients and sidestep common pitfalls. The roadmap typically involves a few key stages.
Phase 1: Assess and Prepare (Months 1-3)
Before making any changes, a clear-eyed assessment is essential. This initial phase is about understanding your starting point. It involves:
- Gauging Readiness: Survey both clinicians and administrative staff to measure their current attitudes toward the shared decision making model. Are they open to it, skeptical, or resistant?
- Identifying Barriers: Pinpoint specific obstacles. Common ones include tight appointment schedules, a lack of private spaces for conversations, and electronic health record (EHR) systems not built for patient-facing interactions.
- Forming a Core Team: Assemble a dedicated team of champions. This group should include clinicians, nurses, administrators, and patient advocates who will guide the implementation. Research shows that diverse teams bring varied perspectives that lead to better results.
Phase 2: Train and Pilot (Months 4-9)
With a solid understanding of the landscape, the next step is to build skills and test the model on a small scale. This prevents organization-wide disruption and allows for refinement.
- Focused Training: Provide practical training on communication techniques, how to use patient decision aids, and ways to manage time efficiently during collaborative conversations.
- Select a Pilot Unit: Choose a single department or clinic—like a primary care practice or a diabetes management center—to test the new workflows. This controlled environment makes it easier to track results and make adjustments.
- Integrate Decision Aids: Introduce evidence-based tools, such as videos, pamphlets, or interactive websites, that help patients understand their options. The goal is to support, not replace, the clinical conversation.
Phase 3: Measure, Refine, and Scale (Month 10+)
The final phase uses data from the pilot program to refine the process before expanding it. Success here depends on both numbers and stories. Key activities include:
- Collect Feedback: Regularly survey patients and providers from the pilot group. Did patients feel more involved? Did clinicians find the new process manageable?
- Analyze Key Metrics: Track outcomes like patient satisfaction scores, adherence to treatment plans, and appointment time usage.
- Gradual Rollout: Based on the lessons learned, fine-tune the training and workflows. Begin expanding the shared decision making model to other departments, one by one. This methodical expansion ensures each new unit is set up for success, creating a sustainable, organization-wide culture of partnership.
To help visualize this journey, the table below outlines the key phases, timelines, and metrics for a successful SDM implementation.
| Phase |
Duration |
Key Activities |
Success Metrics |
Common Challenges |
| 1. Assess & Prepare |
1-3 Months |
- Form a diverse implementation team.
- Survey staff and patient readiness.
- Identify workflow and tech barriers. |
- 75%+ staff survey completion rate.
- Leadership team established and roles defined.
- Barrier report with actionable items. |
- Resistance to change from long-term staff.
- Underestimating time and resource needs. |
| 2. Train & Pilot |
4-9 Months |
- Conduct communication skills training.
- Select a single pilot department.
- Integrate patient decision aids into workflow. |
- 90%+ of pilot staff complete training.
- 20% increase in decision aid usage.
- Positive qualitative feedback from pilot patients. |
- Inadequate training materials.
- Difficulty integrating decision aids with existing EHR. |
| 3. Measure & Scale |
10+ Months |
- Collect patient and provider feedback.
- Analyze data on satisfaction and adherence.
- Create a plan for phased, organization-wide rollout. |
- 15% increase in patient satisfaction scores.
- Measurable improvement in treatment adherence.
- Successful rollout to 2-3 additional departments. |
- Inconsistent application across departments.
- Staff burnout from new process demands. |
This structured approach shows that implementing shared decision making is a marathon, not a sprint. By starting with a thorough assessment, testing on a small scale, and using data to guide expansion, healthcare organizations can build a lasting culture of partnership that benefits everyone involved.
Success Stories That Show What's Possible
The true power of the shared decision making model comes to life when we see it in action. Moving from theory to practice, real-world examples show how this collaborative approach creates better outcomes across diverse medical fields. These aren't just feel-good anecdotes; they are evidence-based case studies showing measurable improvements in patient satisfaction, treatment adherence, and clinical results.
Collaboration in Cardiovascular Care
Cardiovascular medicine is a field where patients often face complex, high-stakes decisions with multiple treatment paths. From choosing between medications with different side effects to deciding on invasive procedures, the "best" path often depends heavily on a patient's lifestyle, risk tolerance, and personal goals. The adoption of shared decision making in cardiovascular care highlights its growing importance, with leading clinical guidelines now recommending this model as a core part of disease management. To explore this further, you can learn how patient involvement is transforming cardiovascular disease management.
Imagine a cardiologist presenting two options for managing high cholesterol: a highly effective statin with a small risk of muscle pain, or a different medication that is slightly less potent but has fewer side effects. Through a shared decision making conversation, the patient—an avid marathon runner—might choose the second option to avoid any risk to their training. This is a crucial personal factor that a purely clinical recommendation might overlook. This collaborative choice respects the patient's priorities, increasing the likelihood they will stick with the treatment plan.
Navigating Difficult Choices in Oncology
Cancer treatment presents some of the most emotionally and medically complex decisions a person can face. The shared decision making model is especially vital here, as it empowers patients to align grueling treatment regimens with their personal values and quality-of-life considerations.
An oncologist might use this model to discuss chemotherapy options with a patient who is also a primary caregiver for their young children. By transparently laying out the different side-effect profiles—one causing severe fatigue, another requiring more frequent hospital visits—the patient can make an informed choice that balances their health needs with their family responsibilities. This process ensures the patient feels in control during a time of immense uncertainty. These kinds of partnerships are essential for success, a principle that applies beyond healthcare. In fact, you might be interested in this SaaS growth co-founder success story, which shows how powerful the right partnership can be.
The Agency for Healthcare Research and Quality (AHRQ) emphasizes the importance of patient experience, which is a core component of this model. The following graphic illustrates the different dimensions that define a positive patient experience.
This visualization shows that a good experience goes beyond clinical outcomes to include communication, respect, and involvement in decisions—all hallmarks of the shared decision making model.
Empowering Autonomy in Mental Health
Mental health is another area where the shared decision making model has proven profoundly effective. Treatment success often hinges on a strong therapeutic alliance built on trust and mutual respect.
By involving patients in choices about therapy types, medication, or lifestyle adjustments, providers honor their autonomy and make use of their self-knowledge. A therapist might work with a client experiencing anxiety to co-design a treatment plan that incorporates mindfulness, exercise, and medication, allowing the client to choose the elements they feel most ready to embrace. This partnership leads to greater engagement and more sustainable mental wellness.
Solving Common Problems Before They Derail Progress
Even the most well-thought-out plans to adopt the shared decision making model can hit predictable snags. While the benefits are clear, real-world challenges can halt progress if you don't see them coming. These hurdles aren’t signs that your approach is wrong; they are the common growing pains that arise when shifting from a top-down system to a collaborative one. By anticipating these issues, your organization can build resilience into its plan and maintain momentum.
One of the biggest obstacles is navigating the human side of change. This involves managing staff resistance and overcoming deeply ingrained habits that can quietly sabotage the best-funded initiatives. This is where creating psychological safety becomes absolutely vital. Just like in any high-performing team, clinicians and staff need to feel secure enough to try new ways of working without the fear of being judged. For leaders, this means fostering an environment where open conversation is the norm. It's a critical lesson for any collaborative project, and you can learn more about its importance by reading our article on founder mental health and building resilient partnerships.
Addressing Time Constraints
The most common objection is time. In a system where appointments are already packed, how can providers find extra minutes for deep, meaningful conversations? It’s a fair question, but it’s often rooted in a misunderstanding. The goal isn't necessarily longer appointments, but more effective ones.
Evidence-based strategies show that shared decision making can actually make better use of time.
- Preparation is key: Giving patients high-quality decision aids—like videos or easy-to-read pamphlets—before their appointment lets them come in with a baseline understanding and thoughtful questions. This front-loading of information makes the face-to-face discussion more focused and productive.
- Structured conversations: Using a clear framework keeps the conversation on track. It ensures all the important points are covered without the discussion wandering off-topic, turning a rambling chat into a goal-oriented dialogue.
When executed properly, a 15-minute collaborative discussion can be far more impactful than a 15-minute monologue. It can prevent the need for follow-up calls and future appointments just to clear up confusion.
Bridging Gaps in Health Literacy
Another significant hurdle is the vast range of health literacy and cultural backgrounds among patients. An approach that works perfectly for one person might be confusing or even inappropriate for another. A successful shared decision making model has to be flexible enough to meet people where they are.
| Challenge |
Solution |
Example in Practice |
| Low Health Literacy |
Use simple language, visuals, and the "teach-back" method. |
A doctor explains a medication and then asks, "To make sure I did a good job explaining, can you tell me in your own words what this is for?" |
| Cultural Differences |
Ask about family involvement and cultural values around health. |
In a culture where family input is crucial, a clinician might ask, "Would it be helpful to have a family member join our next conversation?" |
| Language Barriers |
Use professional medical interpreters, not family members. |
A clinic provides on-demand video interpreting services to ensure communication is accurate, confidential, and respectful. |
Adapting your method while sticking to the core principles of respect and partnership is the key. This flexibility ensures every patient, no matter their background, can be an active partner in their care. True collaboration means tailoring the process, not just the information. By planning for these common issues, healthcare organizations can build strong, adaptable programs that turn potential pitfalls into opportunities for even better patient relationships.
What's Next for Collaborative Healthcare
The shared decision making model isn't a fixed rulebook; it's a living approach that is growing and changing right alongside new technology and what patients have come to expect. As people want more say and transparency in their own care, this partnership model is set for major growth. The future points to a more connected and integrated partnership between patients and clinicians, supported by new tools but always centered on human connection.
A significant area of development is the use of AI-powered decision support tools. These systems are not meant to replace doctors but to help both patients and healthcare providers navigate the increasingly complex web of treatment options. Imagine a tool that takes a patient's unique genetic profile, lifestyle, and personal goals and then projects the potential risks and benefits of various therapies. This elevates the conversation from general statistics to a deeply personal discussion, making the shared decision making model far more precise and effective.
A More Connected and Continuous Dialogue
Another key change is the shift from one-off decisions made during an appointment to a continuous, ongoing collaboration. This is largely made possible by integrating data from wearable devices and patient-reported outcomes.
- Continuous Health Monitoring: Gadgets like smartwatches offer a steady stream of real-world health data, from heart rate variability to sleep quality and activity levels. This information gives providers a much clearer picture of how a treatment is impacting a patient's daily life, paving the way for timely adjustments to the care plan.
- Patient-Reported Outcomes (PROs): These are formal systems where patients can regularly report on their symptoms, quality of life, and ability to function. This creates a direct feedback loop, turning shared decision making into an ongoing conversation rather than a single event.
This constant flow of information transforms the care plan into a living document—one that can be updated collaboratively as the patient's condition and priorities change over time.
Expanding Access Through Technology
Technology is also knocking down geographical walls that have limited access to collaborative care. Telemedicine platforms are making the shared decision making model a reality for people in rural or underserved areas. Patients who once had little access to specialists can now have in-depth, collaborative talks from the comfort of their homes, ensuring they can be active participants in their healthcare journey, no matter where they live.
Even with these exciting technological advancements, the heart of this model is still human. The true aim is to use these tools to strengthen the bond between patient and provider, not to replace it. The best systems will be those that automate administrative work, freeing up more time for meaningful conversation and genuine partnership.
Looking ahead, the focus will also be on improving how we measure the success of these collaborative methods. New research is looking into better ways to quantify patient confidence and satisfaction, while new training programs are helping healthcare professionals master the art of this partnership. We're also seeing policy changes that favor and incentivize care models built on collaboration. These trends all point to a future where shared decision making is not just a nice-to-have, but the standard for excellent, patient-focused care.
Finding the right partner is just as critical in business as it is in healthcare. For solo founders looking to build a strong team, the right co-founder can make all the difference. IndieMerger connects verified entrepreneurs with complementary skills, helping you build a successful startup faster. Stop building alone and find your ideal co-founder on IndieMerger today!